Is the COVID-19 Test Accurate?
Tenzin Gyaltsen (Get Well Clinic)

As Ontario transitions into Stage 3, the province’s COVID-19 testing capacity remains a crucial factor for the speed at which we reopen. Recent numbers may seem promising, coming in at the lowest we’ve seen in months, but how accurate actually are these results? In a recent study by researchers at Johns Hopkins University, COVID-19 test results were shown to be alarmingly inaccurate, particularly in the case of false negatives.
A false negative is defined as a test that comes out negative, but should have been positive. In the case of COVID-19, a false negative refers to a patient that tests negative for their RT-PCR test (Link), but actually does have the virus. It’s easy to imagine why false negative cases are especially dangerous, as sick individuals may feel free to operate and go about their business as they usually do, increasing the risk of community spread.
In the study by Kucirka et al., the probability of a false negative result varied widely, but depended largely on the amount of time after initial exposure that the test was taken. The false negative rate was reported as 100% at the moment of exposure (or Day 0), which may seem drastic but makes sense given the limitations of the test (Link). At this point, the virus would have virtually no time to replicate and so the chances of any viral genetic material being picked up by a cotton swab are little to none. As the days progressed and symptoms developed (around Day 5), the false negative rate decreased to a minimum of 20% (Day 8). Interestingly, after Day 8, the false negative rate began to increase steadily, from 21% on Day 9 to 66% on Day 21. Like the early days of the disease, these high numbers may also be due to the decreased presence of viral genetic material during the patient’s recovery phase.
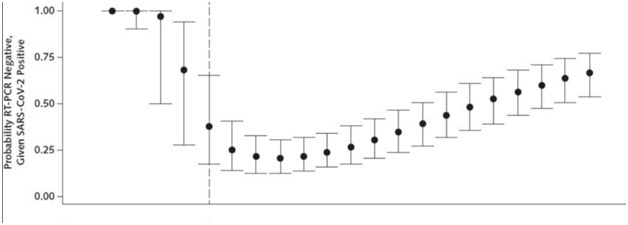
It goes without saying that every study has its own limitations, but the numbers presented in this particular study warrant concern. If we’re to safely continue reopening the province, we should be confident in our testing capability and accuracy, but these findings suggest that the ubiquitous RT-PCR (cotton swab) test may not be enough. It’s not all bad news though. Using the data collected from this study (and similar studies), we may gain a better understanding of when the best time to test patients actually is (i.e. when the false-negative rate is the lowest). From the data presented, it seems like that optimal window is about 2–4 days after symptoms first appear.
There are a number of things we can we take away from this study. The foremost is that the false-negative rate of COVID-19 tests is much higher than one might think, which may lead to an underestimation of the actual number of total cases. If you are feeling sick and receive a negative test result, do not treat it as a definitive answer. Continue to self-isolate to keep the people closest to you safe, and seek medical guidance before taking further steps. If you’re hesitant or unable to to visit a clinic in-person, please contact us (either through the online chat system or call 416.508.5691) to book a virtual appointment!
Source:
Kucirka LM, et al. (2020) Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure. Ann Intern Med. https://doi.org/10.7326/M20-1495



